Dr. Federico Ricci
Fatty liver (metabolic syndrome),
difficulty losing weight, inflamed gut
(dysbiosis, irritable bowel syndrome, diverticular disease).
Gut–liver–brain axis: personalized and monitored nutritional strategy designed to promote well-being and achieve stable, long-term results.

This personalized nutritional program is designed for individuals who recognize themselves in one or more of the following scenarios:
✅ Recurrent intestinal disorders: dysbiosis, irritable bowel syndrome, diverticular disease, persistent bloating, irregular bowel movements.
✅ Inflammation and increased intestinal permeability: symptoms that tend to persist or flare up, with possible immune involvement and autoimmune manifestations.
✅ Dysfunctional metabolic profile: insulin resistance, metabolic syndrome, difficulty losing weight, unstable energy levels.
✅ Fatty liver within an associated metabolic condition: hepatic fat accumulation, altered hormonal signaling (hunger and satiety), and systemic inflammation.
✅ Recurrent migraine and headaches: potential amplification through inflammation and the gut–liver–brain axis.
If you would like to understand whether this program is suitable for your specific situation, you can schedule a free introductory video consultation.
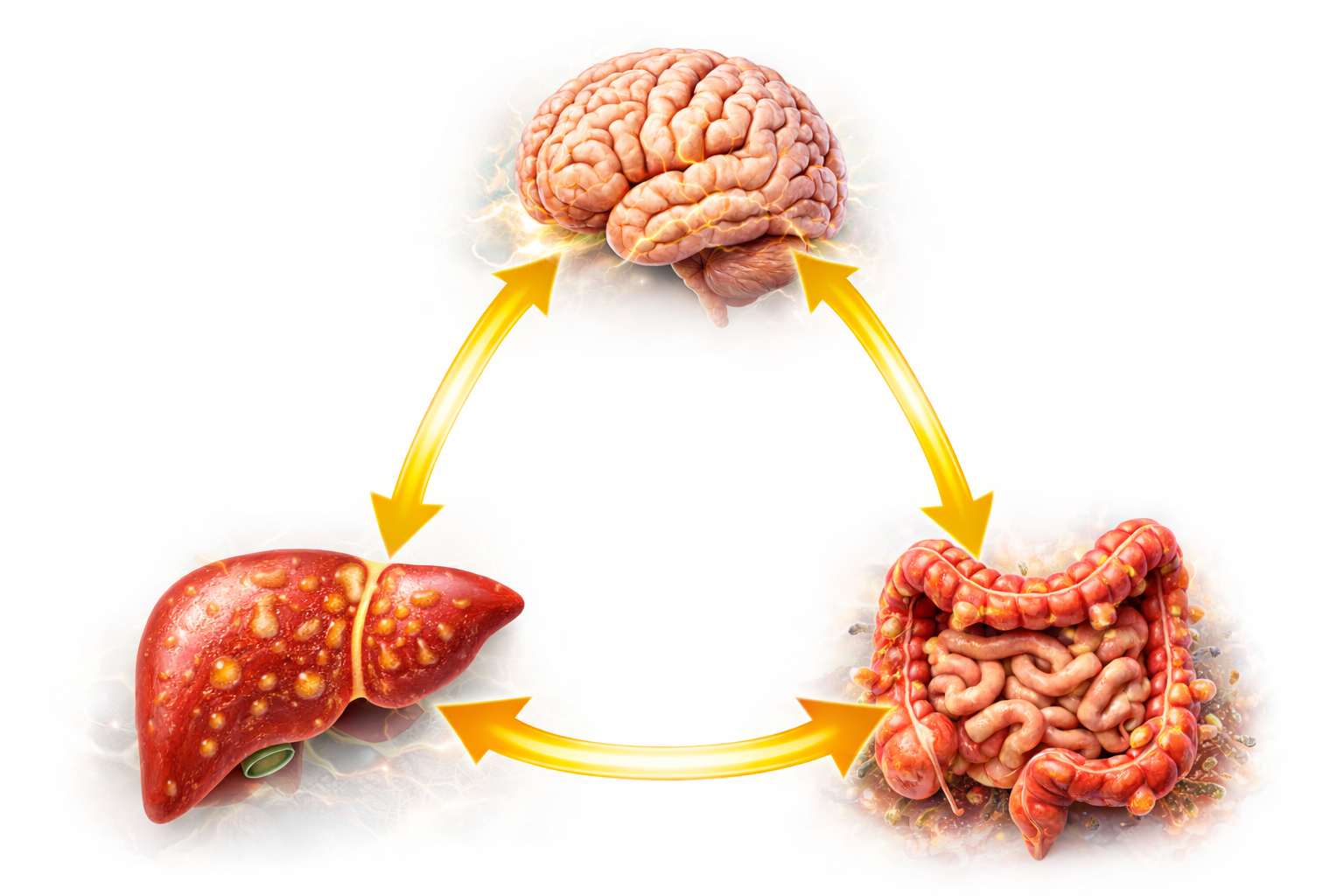
GUT–LIVER–BRAIN AXIS
Today we know that the gut, liver, and brain do not function in isolation: they form a bidirectional axis in which neural signals (via the vagus nerve), hormonal and immune pathways, together with the microbiota and the intestinal barrier,
modulate inflammation, energy metabolism, and appetite regulation.
When this axis becomes dysregulated, symptoms may no longer remain confined to the gut or the liver, but can extend to energy levels, body weight, insulin sensitivity, and neuro-functional symptoms (e.g., headaches, brain fog).
For this reason, a fragmented approach is a mistake: what is required is an integrated, scientifically grounded perspective to build a personalized and monitored nutritional program, targeting inflammation, hormonal signaling, and metabolic response in a precise and structured way.
HOW TO START THE PROGRAM

Click the “SCHEDULE YOUR FREE CONSULTATION” button and request your free introductory video consultation.

Within 24 hours, a member of our team will contact you to gather the essential information and schedule your appointment.

Introductory video consultation: you will describe your specific situation, and I will explain how we work; it is reserved for those who are genuinely interested in undertaking a personalized nutritional program
with ongoing support.
IMPORTANT
The introductory video consultation is free of charge, but it is intended for those who want to undertake a personalized nutritional program with ongoing support over time. If you are looking for quick, generic advice, this is not the right setting: here we establish a tailored nutritional strategy, with weekly follow-up and progressive adjustments based on your individual response over time.
PERSONALIZED NUTRITIONAL PROGRAM WITH ONGOING SUPPORT
The gut, liver, and brain communicate in a continuous and bidirectional manner. This communication occurs through the microbiota, the intestinal barrier, the immune system, inflammatory mediators, hormonal signals, and the vagus nerve. When this axis becomes altered, a single isolated symptom does not simply appear; instead, a self-perpetuating circuit often develops over time. Bloating and bowel irregularity may emerge or worsen, along with difficulty losing weight, dysfunctional hunger and satiety signaling, unstable energy levels, brain fog, headaches, and migraine.
In many cases, the clinical picture is sustained or amplified by insulin resistance, leading to less stable hormonal signaling. The key point is that quality of life may progressively decline if the underlying mechanisms driving the condition are not addressed: low-grade inflammation, dysbiosis, increased intestinal permeability, hormonal dysregulation, and insulin resistance.
Within this context, fatty liver associated with metabolic dysfunction often emerges as well—an expression of hepatic–metabolic overload that tends to further reinforce the cycle.
A personalized and monitored nutritional program is designed to generate, over time, a favorable biochemical and hormonal impact.n The goal is to restore homeostatic balance: to reduce inflammatory burden and immune hyperactivation, improve insulin sensitivity and the regulation of hunger and satiety, and promote more efficient energy production—always tailored to your specific condition and your individual physiological response.
At the epigenetic level, nutrition matters because every meal acts as a signal: it triggers a biochemical and hormonal response that can modulate DNA expression
without altering its sequence.
In practical terms, even with the same genetic background, a targeted nutritional strategy can shift the body toward a profile more compatible with reduced inflammation, improved insulin regulation, and greater coherence of the gut–liver–brain axis over time.
This is why a personalized and monitored nutritional program can be essential: to select and calibrate the right signals over time, in alignment with your symptoms, your goals,
and your daily life.
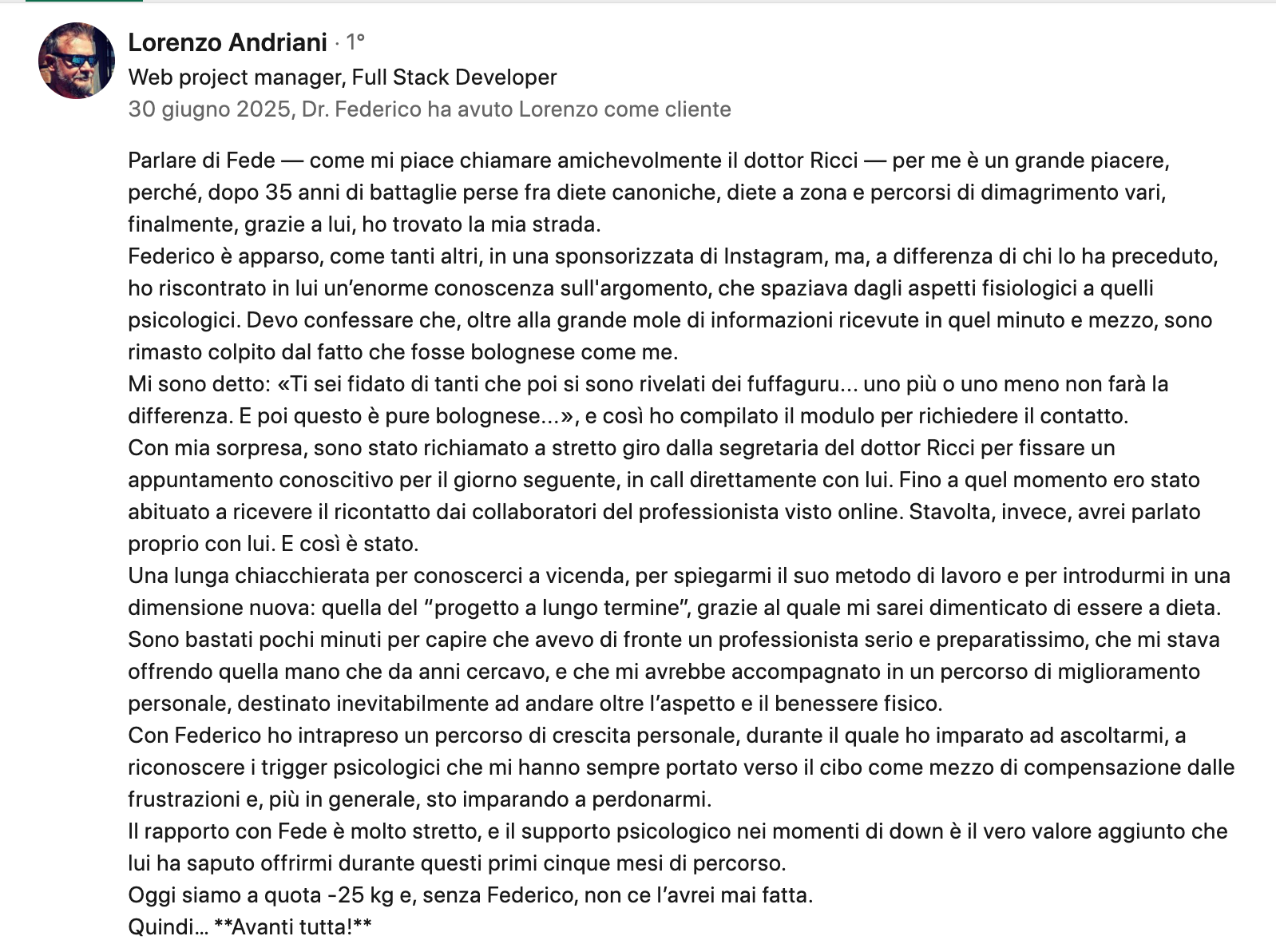
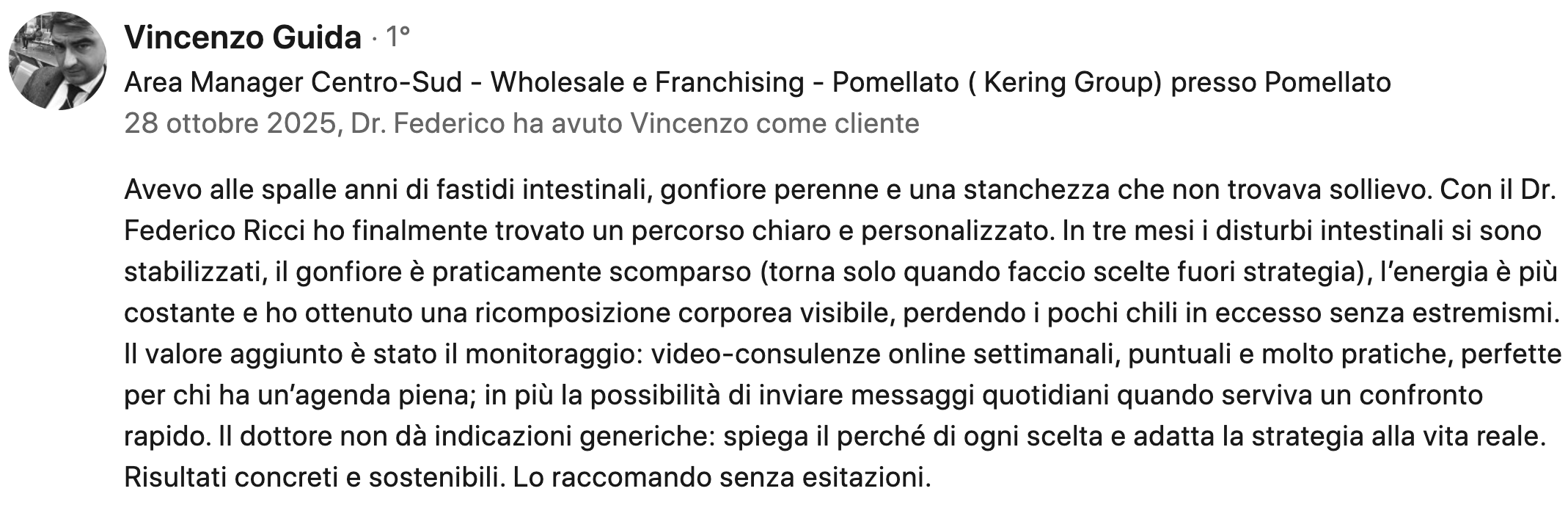
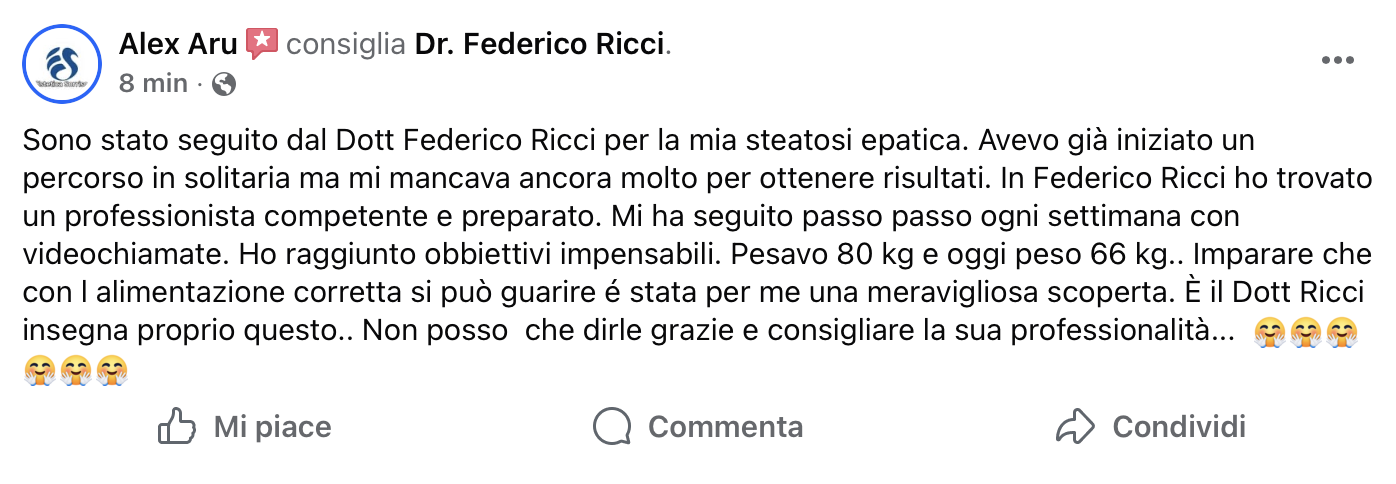
WRITTEN TESTIMONIALS